The patient pathway analysis (PPA) methodology was developed to better understand the alignment between patient care seeking and health service availability. The results can inform programmatic priority setting and planning for more patient-centered availability of services.
The PPA aims to describe the steps TB patients take from the initial point of seeking care to the point of being cured. At the same time, the analysis reviews the availability of TB screening, diagnosis, and treatment at various levels of the health system.
By examining the alignment of care seeking with service availability, the PPA may reveal where TB patients experience delay during care seeking or treatment initiation, access inappropriate care, or are lost to follow-up during their journey toward cure. The intent of the PPA is to help national tuberculosis programs more accurately identify some of the health systems alignment gaps that can be addressed through targeted program interventions.
Background
According to the World Health Organization (WHO), 36% percent of incident tuberculosis (TB) cases in 2017—3.6 million patients —were not notified to National TB Control Programs (NTP). Whether these patients received appropriate diagnosis and treatment or not is unknown. These so-called ‘missing’ cases fall into three groups of patients:
- Patients who never accessed care because of financial, geographic, or other barriers to accessing care.
- Patients who sought care in the private (or non-state) sector and were diagnosed and treated there, but not notified to the NTP.
- Patients who were diagnosed and treated in the public sector but not notified to the NTP.
Finding these ‘missing’ patients is essential, if the goal of ending TB is to be achieved. Patient-centered care is a core principle of the WHO End TB Strategy. Where TB prevention and care services are planned from the top down, according to the available capacities of the health system, there is room to strengthen the patient-centered delivery of services by considering where services should be positioned in order to meet patients based on where they are. Essentially, instead of thinking about ‘where can we provide services?’ patient-centered care asks, ‘where should we position services?’ to most efficiently serve TB patients.
Rationale
The patient pathway analysis (PPA) methodology was developed to better understand the alignment between patient care seeking and TB service availability. The results can inform programmatic priority setting and planning for more patient-centered availability of services.
The PPA aims to describe the steps TB patients take from the initial point of seeking care to the point of being cured. At the same time, the analysis reviews the availability of TB screening, diagnosis, and treatment at various levels of the health system.
By examining the alignment of care seeking with service availability, the PPA may reveal where TB patients experience delay during care seeking or treatment initiation, access inappropriate care, or are lost to follow-up during their journey toward cure. The intent of the PPA is to help tuberculosis programs more accurately identify health systems alignment gaps that can be addressed through targeted program interventions. Figure 1 illustrates a hypothetical patient pathway analysis. This guide addresses each component of the PPA in detail throughout the document.
Alignment with Other Analytical Tools
The PPA is one tool in a suite of analytical tools that can help TB programs better plan for a patient-centered approach to TB care. It has been used to support country planning alongside a number of other analytical tools available from partner organizations such a WHO’s epidemiological analysis and inventory studies, and KIT’s MATCH analysis.
In 2016, the WHO Strategic and Technical Advisory Group (STAG) recommended that WHO, ” Promotes the use of patient pathway analyses in countries to help guide transition to the End TB Strategy and prioritize patient-centred interventions during implementation”. Since this recommendation, the PPA has been implemented as part of several national and sub-national planning exercises, in concert with existing TB analytical approaches.
As a tool to inform TB planning exercises, the PPA provides helpful information about the care-seeking patterns of patients and alignment with service availability. However, additional information about TB services, epidemiology, or patient characteristics are necessary to adequately plan a TB response. Many of these other tools provide further insights these areas. They also bring different analytical techniques such as modeling and geospatial mapping, which add complementary information to that of the PPA.
Objectives
The objective of this document is to explain the process of completing a PPA and interpreting its results for use in programmatic priority setting and planning. Ideally the process of completing a PPA will be done in conjunction with other data analysis activities and will be one of several inputs into the development of strategy and planning documents.
This document provides guidance for anyone involved in TB control who wishes to complete a PPA at a national or sub-national level. Using this document as a guide, readers should be able to:
- Describe how a PPA can support strategy and planning work for TB control
- Describe the PPA methodology
- Identify the best data sources to develop a PPA
- Create a PPA in collaboration with their team, using the PPA wizard
- Interpret the PPA results within the context of programmatic priority setting and planning
Audience
This document is intended for national TB program (NTP) or technical partner staff who support evidence-based decision-making in high-TB-burden settings.
Key Concepts
Defining Health Facility Levels and Sectors
The PPA is built from commonly available population-based surveys and data sets about patient care seeking and service availability. When reviewing data on care seeking and service availability, data sets will often use unique naming conventions that are not standardized across sources. To allow for comparison across sources, the PPA uses a standardized naming convention to organize the data. For each data source, health facility types will be grouped into common categories that will indicate the sector and level of the health to which a facility can be assigned.
The two primary sectors used in the PPA are public and private (or non-state). In many countries, it is useful to split private sector facilities into formal private facilities and informal private facilities, where the informal private facilities include practitioners with little or no formal health training, e.g., drug shops, traditional healers. The designation of non-governmental organizations (NGOs) into public or private sector should align with the country’s norms for categorization.
Categorization may differ by country, reflecting the diversity of health systems. Within each sector category, the PPA groups health facilities into standard levels according to the level of care provided (Figure 2). The standard levels used by the PPA are as follows:
- Level 0 (L0) refers to basic, community-based care. Level 0 services include basic triage, health information, and essential prevention and care. Services are commonly provided as an extension of facility-based care, and are provided by volunteers or paramedical staff with limited formal training. Sputum collection may occur at this level, and L0 staff may serve as treatment supporters for TB patients. Examples: community health worker (public); pharmacies, drug shops, and traditional healers (private).
- Level 1 (L1) refers to a facility that provides primary health care. L1 services are commonly provided on an outpatient basis by nurses, midwives, paramedical staff, or private doctors. Some basic diagnostic services, including basic microscopy and essential medicines, may be available. Rural health centers and private clinics are examples within public and private sector, respectively.
- Level 2 (L2) refers to facilities that provide primary health care as well as more advanced care. L2 facilities commonly have more extensive diagnostic and treatment options and can provide both outpatient and inpatient care. Examples: district hospital (public), rural or NGO private hospital (private).
- Level 3 (L3) refers to facilities that provide specialized care with large inpatient capacity. L3 facilities provide access to specialized doctors and have more sophisticated diagnostic and treatment capabilities. Examples: referral or teaching hospital (public), urban private hospital

Patient Pathway Metrics
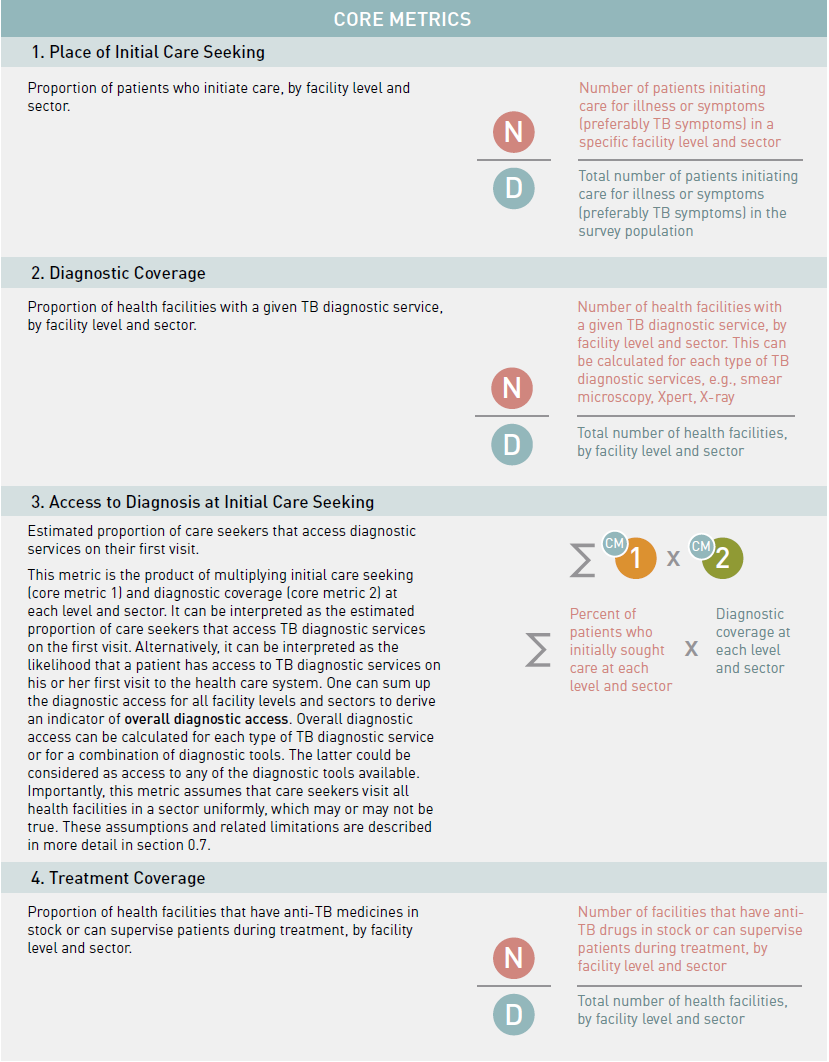
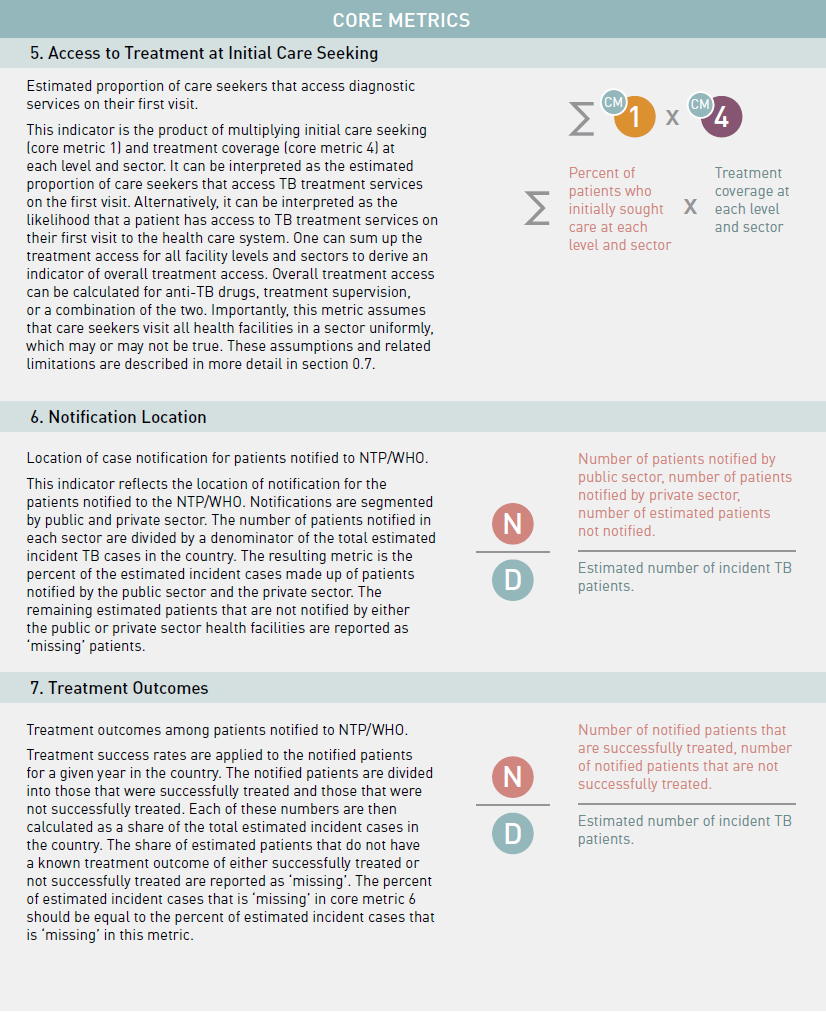
The PPA is intended to present some critical steps patients take on their journey to TB care. To do this, several core metrics are used by the PPA to describe different steps on a patient’s pathway to care. All the core metrics can be segmented by health sector and facility level as described above (Figure 2).
Assumptions and Limitations
When building and interpreting a PPA, it is important that the analysis team keeps in mind several key assumptions and limitations of the PPA. Some teams may have access to data where the appropriateness of these assumptions can be tested for their specific country context, in which case it is highly recommended that the team do so.
Assumption #1 – Care seeking patterns for general illness mirror those for TB-specific symptoms
When countries do not have data on patient care seeking for TB-related symptoms, the PPA will often use care seeking data for general symptoms or other illnesses. As tested in prior PPA case studies, care seeking for a general set of illnesses can be used as a reasonable proxy for TB care seeking. However, in countries where there are unique health systems for a specific illness that are not well integrated in the broader health system, care seeking data for these illnesses should be treated with caution and may not be appropriate to use as a proxy for TB.
Assumption #2 – Health facilities in each sector and level are relatively homogeneous
The PPA metrics described in section 0.6 assume homogeneity across health facilities in each level and sector. Specifically, the underlying assumption suggests that factors like care seeking, lab throughput, or service coverage area are the same across health facilities at each level and sector.
In some cases, this assumption may lead to an overestimation or an underestimation of diagnostic and treatment access at initial care seeking. If PPA teams have access to patient-level records on care seeking or treatment location, they could conduct more detailed analysis to better understand the differences between health facilities.
Assumption #3 – Data sources can be compared across time to help elucidate a patient’s care seeking journey
The PPA uses a wide variety of data sources, which are typically collected at different time periods and from different cohorts. By bringing together these data sources, the PPA can help highlight how patients might move through the health system.
The data sources used for a PPA should be as recent as possible and a time limit should be put on how old the data sources can be. The analysis team should determine a programmatically relevant year in the history of their program and not allow data prior to that point in time to be used. The PPA will then assume that it is reasonable to use data collected after that time and to compare the results of those different data sources.
Additional Limitations
- There is generally a paucity of sub-national data available for care seeking and service availability. When these data are available, if they are further broken down by health facility level and sector, the sample sizes can often become quite small and unsuitable for analysis, making sub-national PPAs more challenging to interpret.
- Unless delay studies are available in the country, the PPA does not provide information on the delay between each step of the pathway. As shown elsewhere, delays in patient care seeking can be an important contributor to the transmission of disease in a community.
- The PPA cannot be used to estimate the drop-offs of a cohort of patients between the steps of a patient’s pathway to care. Other cascade of care studies have been conducted which do provide these estimates and describe the methodology in more detail.
- Finally, the PPA focuses on the availability of services where patients seek care, but it does not try to estimate other factors that may influence whether or not a patient will receive proper care. Other factors, such as the quality of diagnostics and treatment, the capacity of health care workers to provide the service, or the cost of the services may impact whether or not a patient actually is able to receive a necessary TB service at the place they initiate their care seeking journey.